G6PD Deficiency
Key points
- Globally, glucose-6-phosphate dehydrogenase (G6PD) deficiency is the most common enzyme defect.
- All children and youth of Asian, African and Mediterranean descent should be considered for screening for G6PD deficiency upon arriving in Canada, particularly if they had persistent jaundice as newborns.1
- G6PD screening must be done for those at risk before prescribing primaquine (e.g., for malaria) because it is an oxidative trigger.2 Other triggers include sulfa antibiotics and anti-pyretics, infections, naphthalene (mothballs) and fava beans.
- During and shortly after a hemolytic event, the G6PD assay may be falsely normal secondary to reticulocytosis. In such cases, a repeat examination several weeks later may be necessary.
G6PD deficiency
Globally, glucose-6-phosphate dehydrogenase (G6PD) deficiency is the most common enzyme defect. It is predominantly found in African, Middle Eastern and South Asian populations. Only males are affected because the gene that encodes G6PD resides on the X chromosome. Very infrequently, female carriers may have symptoms. The map below shows the prevalence of G6PD deficiency.
Figure 1: Worldwide prevalence of G6PD deficiency
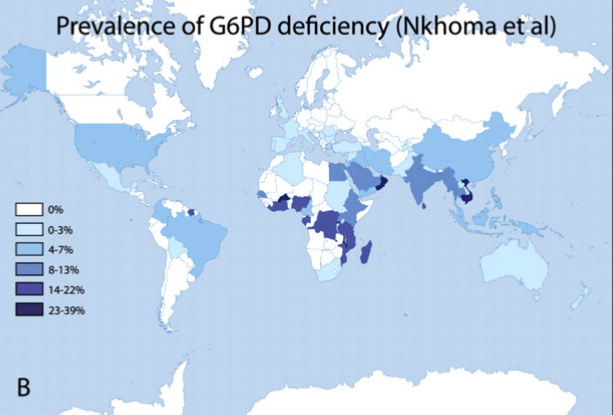
Source: Nkhoma ET, Poole C, Vannappagari V, et al. The global prevalence of glucose-6-phosphate dehydrogenase deficiency: A systematic review and meta-analysis. Blood Cells Mol Dis 2009; 42(3):267-78. With permission.
G6PD deficiency is characterized by decreased levels of the G6PD enzyme, which makes erythrocytes prone to hemolysis when exposed to an oxidative stressor, such as infection, certain drugs or fava beans. Some children with G6PD deficiency present with neonatal jaundice, but many are asymptomatic and can remain undiagnosed until hemolysis is triggered, causing jaundice and sometimes anemia.
Symptomatic episodes are generally self-limited, but may include jaundice, hemoglobinuria, pallor, fatigue, fever, abdominal pain, diarrhea and occasional vomiting. Sometimes, however, the drop in hemoglobin can be severe and a blood transfusion is required. More chronic complications are rare.
Triggers
All children and youth of Asian, African and Mediterranean descent should be considered for screening for G6PD deficiency upon arriving in Canada, particularly if they had persistent jaundice as newborns.1
Primaquine, the malaria drug used to prevent relapse of Plasmodium vivax and P. ovale (for hypnozoite eradication or “radical cure”) is an oxidative trigger. G6PD screening must be done for individuals at risk before prescribing primaquine.2 Many other drugs can trigger hemolytic crisis, including sulfa antibiotics and anti-pyretics (see table). Other triggers include infections, naphthalene (e.g. mothballs) and fava beans. Although patients should be cautioned to avoid these triggers when possible, it should be noted that response to triggers varies among patients and is not always consistent.
Diagnosis
Diagnosis of G6PD deficiency by assay is made to identify reduced G6PD activity in red blood cells. It is important to note that during and shortly after a hemolytic event, the G6PD assay may be falsely normal secondary to reticulocytosis. In such cases, a repeat examination several weeks later may be necessary.
Selected resources
- The Hospital for Sick Children. About Kids’ Health [Handouts]. See What is G6PD Deficiency?
References
- American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 2004;114(1):297-316.
- Committee to Advise on Tropical Medicine and Travel (CATMAT). Canadian recommendations for the prevention and treatment of malaria among international travellers. Can Commun Dis Rep. 2013 In press.
- Jeng M and Vichinksy E. Hematologic problems in immigrants from Southeast Asia. Hematol Oncol Clin N Am 2004;18(6):405-22.
Reviewer(s)
- Andrea Hunter, MD
- Anna Banerji, MD
Last updated: April, 2018
