Providing culturally safety care
Key points
- Health care providers need to be sensitive to differences between their own cultural backgrounds and patients’ backgrounds. Differences in both verbal and nonverbal communication can influence care.
- Culture, religion and ethnicity may influence beliefs and values that people have about health and health care. Both patients and care providers bring their own cultural perspectives to each encounter. Explore a newcomer patient’s or family’s beliefs and values, respecting differences and finding common ground for treatment plans, always in accordance with best practice.
- Although knowing about specific cultures may be helpful, it is also important to avoid overgeneralizing, stereotyping and other culturally based assumptions.
- Do not assume that children and youth from a particular ethnic or cultural group are culturally homogeneous. While culture does influence development and behaviour, there is significant heterogeneity within almost any group. Remember that youth, especially, wish to be seen as individuals.
- In taking a history with a newcomer child, adolescent or family, ask questions that assess sociocultural dimensions, views of health, immigration history, acculturation, identity and religion.
- When there are language barriers between a family and a health professional, using a professional interpreter is recommended.
- By following these suggestions, you will spend considerable time and effort – and probably more than one visit – conducting a history. Consider this an investment in improved health outcomes.
- Providing culturally safe care is critical for improving health outcomes, patient safety and patient satisfaction.
Terminology
Culture
Culture is defined as “the thoughts, communications, actions, customs, beliefs, values, and institutions of racial, ethnic, religious, or social groups”. Culture is present in all patients and care providers, not just immigrant and refugee children, youth and families. Culture plays a role in the interactions among patients, their families, health care providers and systems.
Figure 1
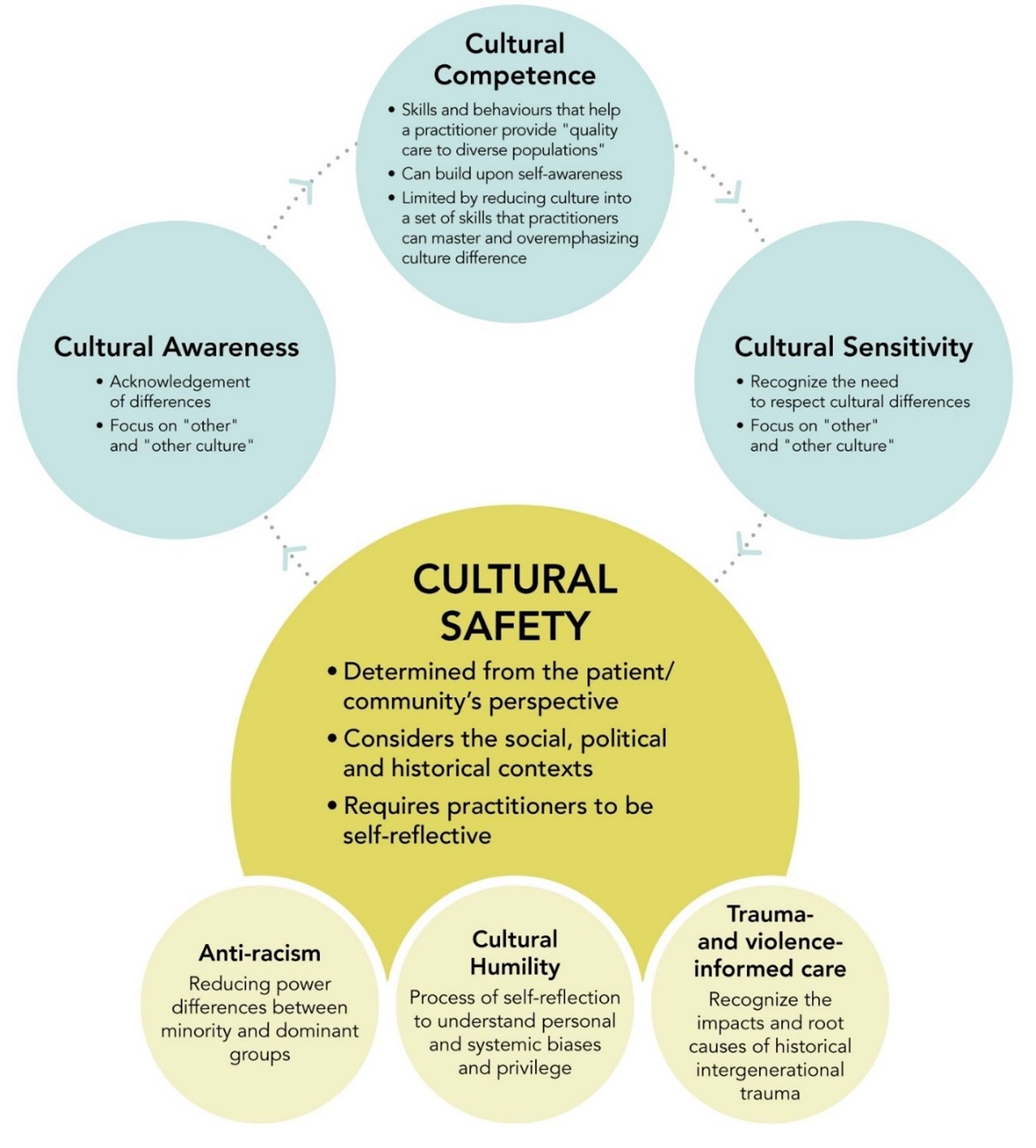
This graphic has been adapted from: Baba, L. (2013). Cultural safety in First Nations, Inuit and Métis public health: Environmental scan of cultural competency and safety in education, training and health services. Prince George, British Columbia, Canada: National Collaborating Centre for Indigenous Health. BC First Nations Health Authority. "Cultural Humility." 2019; Brascoupé, S. and Waters, C. (2009). Cultural safety: Exploring the applicability of the concept of cultural safety to Aboriginal health and community wellness. Journal of Aboriginal Health. Retrieved from: © All rights reserved. Common Definitions on Cultural Safety -- CPHO's Health Professional Forum. Public Health Agency of Canada, 2023. Reproduced with permission from the Minister of Health, 2024. Available at: definitions-en2.pdf
Cultural safety
Cultural safety (see Figure 1) is the ultimate goal in a learning process, according to Irihapeti Ramsden, the Maori nurse and educator who developed the concept. It starts with awareness of a patient’s ethnicity or community and, in culturally safe practice, growing concerns with “social justice ... and nurses’ power, prejudice and attitude”.
Cultural safety puts the experience of the patient at the centre of the clinical encounter. Only a patient can determine whether a health care experience has been culturally safe. Cultural safety is an outcome that requires health professionals to engage respectfully with patients, and to recognize and try to address power imbalances in the healthcare system. For people to feel safe in the health care system, health professionals need to work to create an environment free of racism and discrimination.
The LEARN model is one framework for learning to provide culturally safe care that is action- oriented and focuses on what health care providers can do.
- Listen with sympathy and understanding to the patient’s perception of a problem
- Explain your perceptions of a problem
- Acknowledge and discuss differences and similarities
- Recommend treatment
- Negotiate agreement
Cultural humility
Cultural humility expands on cultural competence by emphasizing a lifelong commitment to self-evaluation, self-critique, awareness of one’s own implicit or explicit biases, and managing inherent power imbalances related to culture. Here are some actions to help health care practitioners develop cultural humility:
- Focus on the patient during interviews, and listen for the way patients talk about themselves.
- Talk to patients using a less controlling and authoritarian style, using interactive communication. This approach tells patients that their own agenda and perspectives (biomedical and non-biomedical) are valued.
- Realize that you do not need to understand every group’s health beliefs. Encourage individual patients to communicate how much or how little their culture has to do with an issue.
- Be aware of the cultural differences between yourself and your patients. Being aware helps to avoid conflict during diagnosis or while developing a treatment plan.
- Critically examine, and bring awareness to, your own culturally influenced beliefs and biases as they arise in clinical encounters.
- Allow patients to take on the role of expert themselves and become true partners in determining the care they receive.
- As needed, guide patients about social and cultural norms or customs in Canada. To inform isn’t to blame or humiliate, it’s to respect the newcomer as a learner. There are issues where stronger guidance may be needed (e.g. around a practice like female genital cutting). If a tradition conflicts with Canadian laws or human rights, be sure to let the patient know.
Why cultural safety is important
Given Canada’s increasingly diverse population, it’s important for health professionals to provide culturally safe care. Culturally safe care helps to reduce disparities and improve health outcomes in a diverse population by improving communication and helping to effectively manage cultural differences, including beliefs about health and health practices, as part of patient care.
Culture, religion and ethnicity may influence people’s beliefs and values about health and health care, and both patients and providers bring cultural perspectives to each encounter. Areas where different perspectives can affect clinical care include:
- Birth and early infant care practices
- Nutrition and diet
- Bedsharing and Sudden Infant Death Syndrome
- Developmental disabilities
- Parenting and discipline
- Adolescent issues, including development, confidentiality, roles within the family and/or extended family, sexuality, substance use and other risky behaviours, identity development and acculturation
- Accessing health care systems, clinics and emergency departments
- Using traditional medicines and treatments
Read more about how culture influences health here.
Caught in the middle
A case that illustrates the importance of cultural competence is documented in Anne Fadiman’s book, The Spirit Catches You and You Fall Down—A Hmong Child, Her American Doctors, and the Collision of Two Cultures.
This book explores a conflict over care between a small California county hospital and a refugee family from Laos. Lia Lee was a child diagnosed with severe epilepsy whose health care providers and family had very different, culturally rooted health beliefs and
understandings of this condition. Disagreement over appropriate treatment led to Lia being placed in foster care by petition of her doctors. She was later returned to her family but a seizure left Lia in a persistent vegetative state at four years of age.
Her parents and her doctors both wanted what was best for Lia, yet their lack of mutual understanding led to tragedy. The following quotes are lessons learned by health care providers acquainted with the case:
- “I look at patients holistically and acknowledge the fact that developing a treatment plan requires incorporating complementary interventions based on cultural practices and beliefs. I have learned, especially in working with the elderly, how much family can help with the compliance issue.”
- “I think most providers now realize that the mind and body work together. Many people from many cultures believe in the important role that spirituality plays in healing. In fact, in this matter, we are not unlike our Asian patients. Finding an opportunity to engage patients, their families and their communities in spiritual activities is helpful. When it is appropriate, I often encourage the use of rituals such as ‘soul calling’ and/or Buddhist chants (prayers). We encourage families to bring Buddhist monks to the medical center for prayers.”
Working with newcomer children and adolescents
When working with immigrant and refugee children, youth and families, health care providers need to be mindful of their own general approach to care, of including cultural issues in history-taking, and of involving cultural aspects in treatment planning and anticipatory guidance. Health care providers need to be sensitive to differences between their own cultural background and a newcomer patient’s background. Differences in both verbal and nonverbal communication can influence care.
General approaches to care
- Assess your own biases and values. Self-awareness is as important as understanding a newcomer patient’s or family’s background.
- Understand and consider the patient’s agenda.
- Show respect by acknowledging and validating a patient’s or family’s personal and cultural strengths, their resilience in surviving adverse experiences and their ability to adapt to a new culture.
- Determine the patient’s understanding of and explanations for a health condition or illness.
- Project an attitude of curiosity—the patient becomes the teacher and the provider becomes the student.
- Arrange for an interpreter to be present if needed and possible.
By following these suggestions, you may spend considerable time and effort – and probably more than one visit – conducting a history. Consider this an investment in improved health outcomes. Read about medical assessments for newcomer children.
Taking a history
To ensure that culture is included in a child’s or youth’s history, consider asking the following questions:
Assess immigration history and possible immigration stress or trauma.
-
What is your country of origin? What ethnic group(s) do you identify with? What language(s) do you speak? What is the main language spoken in your home? What language do you prefer speaking?
-
Why and when did you come to Canada? How did you arrive in this country? What were some of the challenges and difficulties? What helped you and your family adjust and cope with these challenges?
 Acculturation relates to the change in the culture of a group or the change in the psychology of an individual in response to a new environment or other factors. Adaptation is the process of change in response to a new environment and is one component of acculturation. Learn more about acculturation and its importance to health.
Acculturation relates to the change in the culture of a group or the change in the psychology of an individual in response to a new environment or other factors. Adaptation is the process of change in response to a new environment and is one component of acculturation. Learn more about acculturation and its importance to health.
Assess identity development and acculturation, and potential acculturation gaps and conflicts within families.
- What is causing you stress or difficulty? Do you have a support system? Have you made contact with local cultural associations?
- Is your entire family in Canada? If you left family members behind, are they safe? How do you communicate with them?
- Do you feel more comfortable being with people of your family’s background, or mainstream Canadian society, or both, or neither?
- Do the parents and children in the family speak the same primary language? Who speaks English or French? How well can you speak and read English or French? Do you ever interpret for your parents?
- Do you know how to communicate by telephone? By electronic or social media?
- Who makes meals? Who cares for younger siblings?
- Are you in school yet? How do you like it? How many days do you miss? What are your hopes for the future?
- Have you made friends? Name your best friend. Where do you play with your friends? Do your friends visit you at home?
Explore sociocultural dimensions of health and health beliefs. This will help with negotiating a treatment plan.
- What do you think has caused this problem? What do you call it? How do you understand it?
- Have you had this problem before? How was it treated before? What do you believe will cure this problem?
- How does it affect your life (your child’s life)?
- What do you fear most about this problem? Are you afraid of being excluded from your own community because of this problem? (e.g., tuberculosis, a disability or a congenital abnormality)
- Is there anything else you want to tell me, about this situation or your family or culture that will help me provide you with better care?
Recognize the role of traditional, complementary and alternative medicine.
- What kind of treatment do you think would work? Are there any healing practices or medicines that are traditional for your family that you think might help? Is there anything that may help you to feel better that doctors may not know about?
- Who helps you to handle health issues?
Ask about bias, racism or discrimination.
Recognize that newcomer children and adolescents often experience bias, racism or discrimination in their school or neighbourhood. Such encounters can have a negative impact on development, mental health, family relationships and health behaviours. Ask about these experiences as part of the social history, validate them, and provide appropriate counselling or referrals to mental health and community agencies.
- Some other children (young people) with the same background have told me about being teased, bullied or harassed, just because of their background or the way they look. Has that ever happened to you?
- Do you play outside? Walk to school? Do you ever get scared going to school or playing? Please explain it to me.
Screen all adolescents equally for risky behaviours, such as sexual activity or substance use.
Never assume that adolescents from a particular cultural group are more or less likely to adopt a behaviour than someone from another group.
Treatment planning and anticipatory guidance
To involve culture in a newcomer patient’s treatment, take the following steps:
- Respect that a patient’s or family’s health beliefs may differ from a biomedical model of disease etiology and treatment. Demonstrate compassion by respecting cultural beliefs and practices (for example, traditional therapies).
- When differences arise, try to negotiate a treatment plan to create a shared understanding for treatment. This may include traditional treatments. Emphasize common goals (e.g., helping your child get better), while acknowledging differences. Use patient-centred, collaborative, respectful approaches, balancing compromise and flexibility with medical safety and ethical considerations. For more examples and discussion on negotiating a treatment plan, see J. Campinha-Bacote’s 2011 article on cultural competency.
- Acknowledge and explain the limitations of Canadian health and education systems.
- Explain access to paramedical services, child care, and other educational or supportive services in your area.
- Each newcomer will adapt to Canada in their own way and the nature of this relationship will change over time. Acculturation and identity development are dynamic processes.
Selected resources
- Ball, J. (2008). Promoting cultural safety in child and family services. Poster presentation at The Biennial Early Years Interprofessional Conference (Poster).
- Berry JW. Acculturation: Living successfully in two cultures. IJIR 2005;29(6):697- 712.
- Betancourt JR, et al. Cultural competence and health care disparities: Key perspectives and trends. Health Aff 2005;24(2):499-505.
- Brascoupé S, Waters C. Cultural safety: Exploring the applicability of the concept of cultural safety to Aboriginal health and community wellness. J Aboriginal Health 2009;5(2)6-41.
- Cainha-Bacote J. Delivering patient-centered care in the midst of a cultural conflict: The role of cultural competence. Online J Issues Nurse 2011;16(2):5.
- Canadian Nurses Association. Position statement: Promoting cultural competence in nursing, 2018.
- Canadian Paediatric Society (Caring for Kids New to Canada Task Force). Access to appropriate interpretation is essential for the health of children. (). Paediatr Child Health 29(1):43-45.
- Common Definitions on Cultural Safety: Chief Public Health Officer Health Professional Forum, Public Health Agency of Canada, 2023.
- Fadiman, A. The spirit catches you and you fall down: A Hmong child, her American doctors, and the collision of two cultures. New York: Farrar, Straus and Giroux, 1997.
- First Nations Health Authority. Cultural Safety and Humility.
- Georgetown University. National Center for Cultural Competence.
- Ramsden IM. 2002. Cultural safety and nursing education in Aotearoa and Te Waipounamu. Thesis: Victoria University, Wellington, New Zealand.
- Society of Obstetricians and Gynaecologists of Canada. Guideline No. 395-Female Genital Cutting, Journal of Obstetrics and Gynaecology Canada, Volume 42, Issue 2, 2020, Pages 204-217.e2.
Reviewer(s)
Shazeen Suleman, MD
Last updated: November, 2024
